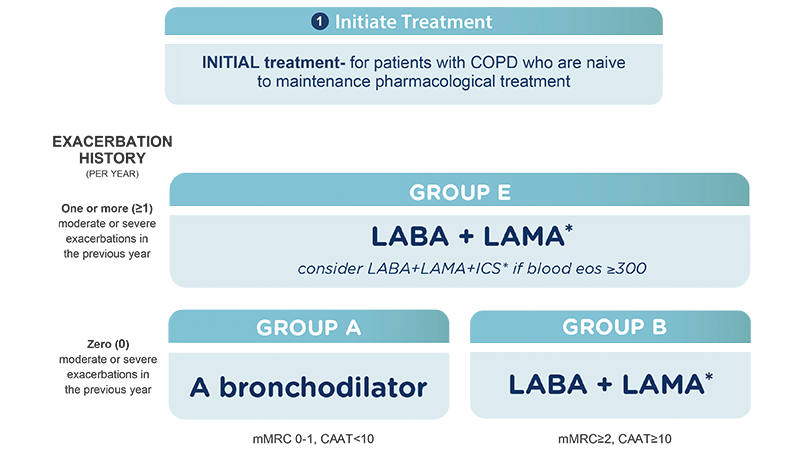
GOLD recommends LABA/LAMA therapy as the preferred way to initiate treatment for patients in both Group B and Group E1
-
*
Single inhaler therapy may be more convenient and effective than multiple inhalers; single inhalers improve adherence to treatment. Exacerbations refers to the number of exacerbations per year; eos: blood eosinophil count in cells per microliter; mMRC: modified Medical Research Council dyspnea questionnaire; CATTM: Chronic Airways Assessment TestTM.
Adapted from © 2025, 2026 Global Initiative for Chronic Obstructive Lung Disease, Inc. Available from www.goldcopd.org.
Learn more about using LAMA/LABA in COPD from the Chair of the GOLD Science Committee
GOLD, Global Initiative for Chronic Obstructive Lung Disease; LAMA, long-acting muscarinic antagonist; LABA, long-acting beta2-agonist; ICS, inhaled corticosteroid.
STIOLTO® RESPIMAT® (tiotropium bromide and olodaterol) Inhalation Spray is a combination of tiotropium, an anticholinergic, and olodaterol, a long-acting beta2-adrenergic agonist (LABA), indicated for the long-term, once-daily maintenance treatment of patients with chronic obstructive pulmonary disease (COPD), including chronic bronchitis and/or emphysema.
Important Limitations of Use
STIOLTO is NOT indicated to treat acute deterioration of COPD and is not indicated to treat asthma.
CONTRAINDICATION
Use of a LABA, including STIOLTO RESPIMAT, without an inhaled corticosteroid (ICS) is contraindicated in patients with asthma.
STIOLTO is contraindicated in patients with hypersensitivity to tiotropium, ipratropium (atropine derivatives), olodaterol, or any component of this product.
In clinical trials and postmarketing experience with tiotropium, immediate hypersensitivity reactions, including angioedema (including swelling of the lips, tongue, or throat), itching, or rash have been reported. Hypersensitivity reactions were also reported in clinical trials with STIOLTO.
WARNINGS AND PRECAUTIONS
LABA as monotherapy (without an ICS), for asthma increases the risk of asthma-related death, and in pediatric and adolescent patients, increases the risk of asthma-related hospitalizations.
Do not initiate STIOLTO in patients with acutely deteriorating COPD, which may be a life-threatening condition, or used as rescue therapy for acute symptoms. Acute symptoms should be treated with an inhaled short-acting beta2-agonist.
STIOLTO should not be used more often or at higher doses than recommended, or with other LABAs as an overdose may result.
If immediate hypersensitivity reactions occur, such as urticaria, angioedema, rash, bronchospasm, anaphylaxis, or itching, discontinue STIOLTO at once and consider alternative treatment. Patients with a history of hypersensitivity reactions to atropine or its derivatives should be closely monitored for similar hypersensitivity reactions to STIOLTO.
If paradoxical bronchospasm occurs, discontinue STIOLTO immediately and institute alternative therapy.
STIOLTO can produce a clinically significant cardiovascular effect in some patients, as measured by increases in pulse rate, systolic or diastolic blood pressure, and/or symptoms. If such effects occur, STIOLTO may need to be discontinued.
Use caution in patients with convulsive disorders, thyrotoxicosis, diabetes mellitus, ketoacidosis, in patients with known or suspected prolongation of the QT interval, and in patients who are unusually responsive to sympathomimetic amines.
Use with caution in patients with narrow-angle glaucoma. Instruct patients to contact a physician immediately if signs or symptoms of acute narrow-angle glaucoma develop.
Use with caution in patients with urinary retention especially in patients with prostatic hyperplasia or bladder-neck obstruction. Instruct patients to consult a physician immediately should any of these signs or symptoms develop.
Patients with moderate to severe renal impairment (creatinine clearance of <60 mL/min) should be monitored closely for anticholinergic side effects.
Be alert to hypokalemia and hyperglycemia.
ADVERSE REACTIONS
The most common adverse reactions with STIOLTO (>3% incidence and higher than an active control) were: nasopharyngitis, 12.4% (11.7%/12.6%), cough, 3.9% (4.4%/3.0%), and back pain, 3.6% (1.8%/3.4%).
DRUG INTERACTIONS
Use caution if administering adrenergic drugs because sympathetic effects of olodaterol may be potentiated.
Concomitant treatment with xanthine derivatives, steroids, or diuretics may potentiate any hypokalemic effect of olodaterol.
Use with caution in patients taking non–potassium-sparing diuretics, as the ECG changes and/or hypokalemia may worsen with concomitant beta-agonists.
The action of adrenergic agents on the cardiovascular system may be potentiated by monoamine oxidase inhibitors or tricyclic antidepressants or other drugs known to prolong the QTc interval. Therefore, STIOLTO should be used with extreme caution in patients being treated with these drugs. Use beta-blockers with caution as they not only block the therapeutic effects of beta-agonists, but may produce severe bronchospasm in patients with COPD.
Avoid co-administration of STIOLTO with other anticholinergic-containing drugs as this may lead to an increase in anticholinergic adverse effects.
STIOLTO is for oral inhalation only.
The STIOLTO cartridge is only intended for use with the STIOLTO RESPIMAT inhaler.
Inform patients not to spray STIOLTO into the eyes as this may cause blurring of vision and pupil dilation.
CL-STO-100021 6.5.2019
Please see full Prescribing Information, Patient Information, and Instructions for Use for STIOLTO RESPIMAT.
Reference
-
Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. Accessed, December 02, 2025. https://goldcopd.org/2026-gold-report.


